Cervical Cancer: Recognising the Signs and Symptoms
Cervical cancer is one of the most common female cancers in the UK, with over 3,000 cases being diagnosed each year, of which more than 25% lose their lives1. Approximately 60% of those affected by cervical cancer will survive 5 years or more; if diagnosed early, the survival rates of cervical cancer will be significantly better when treatment is far more successful and effective. In addition, unlike many other types of cancer, abnormal cell changes in the cervix can in fact be detected and treated before they can even have the chance to develop into cancer.
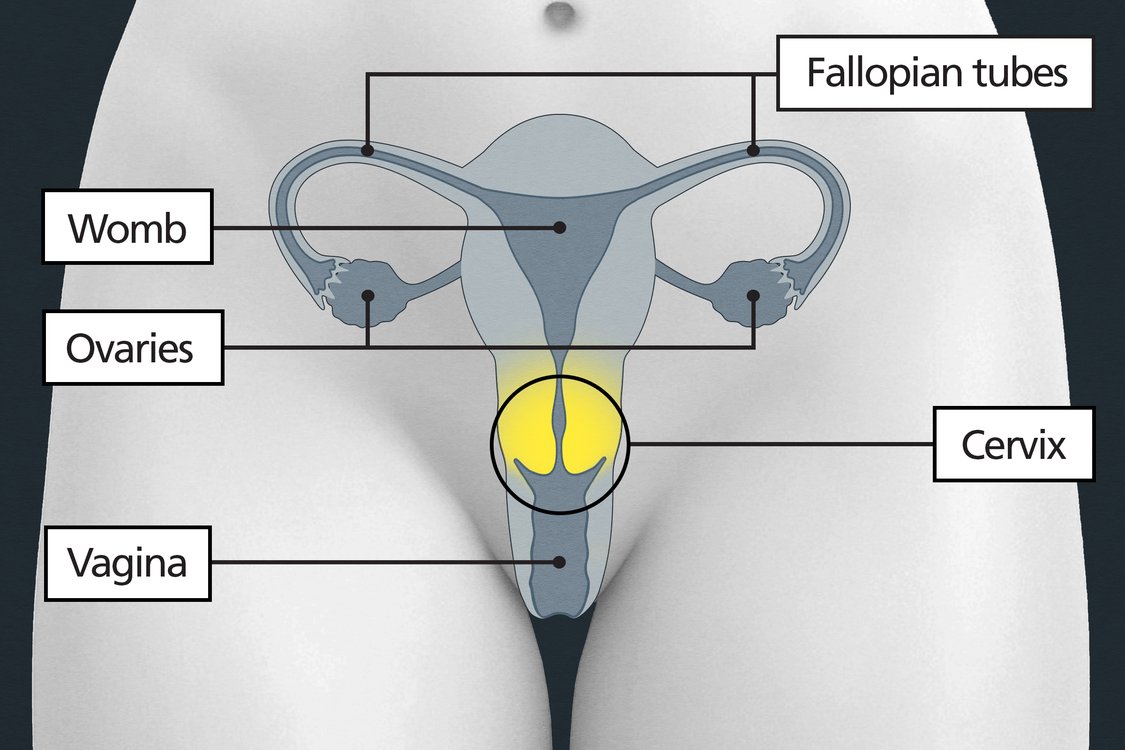
Figure 1 The female reproductive system2
Early diagnosis
Virtually all (99.8%) of cervical cancer cases are caused by high-risk human papillomavirus (hr-HPV) infection1. This makes cervical cancer a preventable disease by implementing certain measures aimed at the early detection of HPV and close monitoring, which, in addition to helping prevent cervical cancer, can potentially lead to its ultimate elimination3.“Early diagnosis is incredibly important with cervical cancer. As we screen for hr-HPV, we can identify those at risk before cell changes even happen. Technically, this could result in cervical cancer being one of the first cancers to be eliminated, and we can definitely get the numbers of those affected down” explains Dr. Angela Pine, 10zyme’s Founder and CEO.
Cervical screening programme
The UK’s NHS cervical screening programme invites women and people with a cervix aged 25-49 years old for screening every three years, and those aged 50-64 every five years4. Since 2019, samples taken from the cervix are screened for the presence of high-risk HPV; a positive HPV diagnosis will lead to further testing to check for abnormal cell changes, and a follow-up appointment is scheduled to ensure that the infection has cleared up or whether there are any persisting cell changes, in which case early intervention would be necessary.
Under 25s
Those who are under the age of 25 are not routinely offered cervical screening. This is because the risk of developing cervical cancer in this age group is very rare as it represents only less than 1% of all cases5. Additionally, research suggests that the risks of offering cervical screening for those under the age of 25 outweigh the benefits and that cell changes in the cervix are quite common during this particular period in life, which usually clear up on their own without any intervention. However, if you are under 25 and experience any possible signs or symptoms of cervical cancer, it is very important to see your GP as soon as possible in order to rule out serious health conditions.
Problems with cervical screening
Although screening is an incredibly effective way of detecting and/ or preventing cervical cancer, according to the latest report released by England’s NHS Cervical Screening Programme for the years 2022-2023, uptake of cervical screening remains low with only 68.7% of eligible individuals aged 25 to 64 adequately screened, a figure that has actually decreased by 1.2% compared to the previous year6. This is caused by a number of different factors that act as ‘barriers’ to cervical screening.
Many reasons exist for not attending cervical screening appointments. This could be because of the invasive nature of the test itself, which often leaves many individuals feeling too uncomfortable or embarrassed to go through with the actual procedure. Some may not attend their appointments due to issues relating to inconvenience, because they would have to take time off work or from their daily routine in order to do the test; or it could be due to problems with access to appropriate healthcare providers. All this highlights the urgent need to improve the processes involved in existing cervical screening to increase its uptake among the eligible population. The aim will be to boost early detection rates of HPV infection and/ or abnormal cell changes and ultimately prevent the development of cervical cancer.
Cervical cancer symptoms
HPV, the virus that causes the majority of cervical cancer cases, often does not cause any symptoms at all. This means that you can carry the virus and pass it on to another person without even being aware. Additionally, cervical cell changes and the associated cancer can take years to develop. This underscores the importance of early detection of HPV infections, in addition to the close monitoring and early intervention of cases, for the effective prevention of cervical cancer.
One reason for the relatively high mortality rate from cervical cancer is that during its early stages, it is often not associated with any signs or symptoms; this means that these usually appear only once the cancer has reached a more advanced stage when treatment is likely to be more challenging. The following are the most common symptoms of cervical cancer7:
-
- Unusual vaginal bleeding – This includes bleeding during or after sexual intercourse, bleeding between periods, heavier and longer periods than usual, or bleeding after menopause.
- Unusual vaginal discharge – While it is normal for women to develop some vaginal discharge that may change in appearance or texture over the course of the month, watery or bloody discharge that is unusual can possibly be caused by cervical cancer.
- Pelvic/ lower abdominal pain – While this can have a number of causes, pelvic pain that has no obvious cause, especially when it persists for a long period, may be a symptom of cervical cancer.
- Lower back pain – As with pelvic pain, long-lasting back pain of no apparent cause could also be a result of cervical cancer.
- Pain during sexual intercourse – For some women, pain or discomfort during sex is a frequent experience. However, cervical cancer can result in the experience of a new type of pain or a change in its intensity “Some people experience pain during sex regularly. We are looking for changes – anything outside the norm” explains Dr. Angela Pine.
It is important to know that the above symptoms could also be caused by other much more common gynaecological conditions e.g. fibroids or endometriosis. Nevertheless, it is essential to visit the GP whenever something feels out of the ordinary or if there is ever any suspicion or doubt because if the symptoms were actually found to be caused by cancer, finding it early means that treatment would likely be much more effective.
Conclusion
In summary, women know their own bodies very well and are usually good at telling when something is wrong. However, often there is a significant challenge in prioritising health adequately. It is important to maintain a mindset that focuses on one’s own well-being, which includes being aware of the symptoms of cervical cancer and knowing when to seek medical advice if there is any reason for concern. Although investigating any symptoms related to cervical cancer is crucial, preventative measures with HPV vaccination and cervical screening can prevent cancer from progressing to a stage where symptoms are detected.
10zyme: Advancing women’s health
We’re developing a groundbreaking self-test with instant results to detect the main cause of cervical cancer: high-risk HPV. Detecting infections early prevents cancer ever developing.
By enabling self-testing, we aim to empower women, overcome stigma and anxiety, and help eliminate a disease killing hundreds of thousands a year globally. See our Education Section to find out more.
Please follow and support us on social media: LinkedIn, Instagram, and TikTok.
References:
-
- Cancer Research UK (CRUK). (2015-2018). Cervical cancer statistics. [Online]. Available at: https://www.cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/cervical-cancer [Accessed 20/03/2024]
-
- National Health Service (NHS). (2021). Overview: Cervical cancer. [Online]. Available at: https://www.nhs.uk/conditions/cervical-cancer/ [Accessed 20/03/2024]
-
- National Health Service of England (NHS England). (2023). NHS sets ambition to eliminate cervical cancer by 2040. [Online]. Available at: https://www.england.nhs.uk/2023/11/nhs-sets-ambition-to-eliminate-cervical-cancer-by-2040/ [Accessed 21/03/2024]
-
- National Health Service (NHS). (2022). What is cervical screening? [Online]. Available at: https://www.nhs.uk/conditions/cervical-screening/what-is-cervical-screening/ [Accessed 21/03/2024]
-
- Jo’s Cervical Cancer Trust. (2019). Cervical screening aged 24 or under. [Online]. Available at: https://www.jostrust.org.uk/information/cervical-screening/cervical-screening-under25 [Accessed 22/03/2024]
-
- National Health Service of England (NHS England). (2023). Cervical Screening Programme, England – 2022-2023. [Online]. Available at: https://digital.nhs.uk/data-and-information/publications/statistical/cervical-screening-annual/england-2022-2023 [Accessed 23/03/2024]
- National Health Service (NHS). (2021). Symptoms: Cervical cancer. [Online]. Available at: https://www.nhs.uk/conditions/cervical-cancer/symptoms/ [Accessed 23/03/2024]