Women’s Health: Understanding Cancers of the Female Reproductive System
The female reproductive system is a complex network of organs and structures, each with its own unique roles and features. This includes the ovaries, fallopian tubes, uterus, cervix, vagina, and external genitalia (vulva).
In this article, we will focus on three parts of the female reproductive system – the cervix, vagina, and vulva, shedding light on their unique roles in women’s health and how infection with human papillomavirus (HPV) can lead to the development of cancer in these bodily regions.
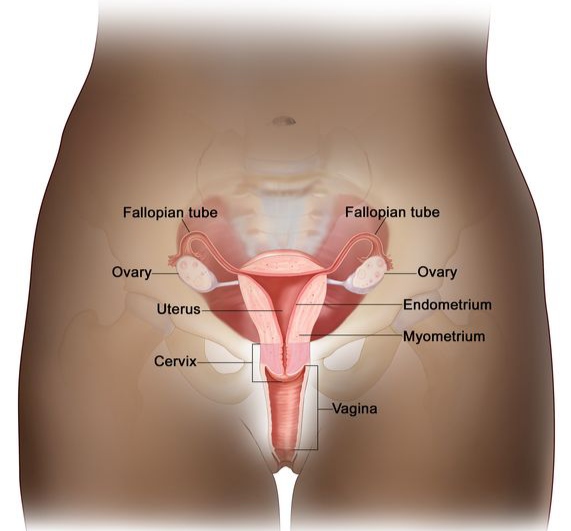
Figure 1 Anatomy of the female reproductive system1
Cervix
The cervix is the lower narrow part of the uterus that connects the vagina (birth canal) to the upper part of the uterus2. It plays a number of crucial roles in women’s health, including fertility, pregnancy, menstruation, and childbirth, in addition to forming an important barrier for protecting the reproductive organs, particularly the uterus, against infections3. Regular cervical screenings are crucial for ensuring the optimal health of the cervix by helping in the early detection of any abnormalities, including reducing the risk of cervical cancer.
Vagina
The vagina, commonly known as the birth canal, is the muscular tube that connects the cervix to the vulva. It provides an important passageway for the penis during sexual intercourse, menstrual flow during menstruation, and newborn during childbirth. Additionally, it plays an essential role in the defence against infections due to its acidic pH4.
Vulva
The vulva refers to the folds of skin between the legs, representing the external part of the female genital area. It includes several structures such as the labia majora and minora (the outer and inner ‘lips’), clitoris, and the vestibule which contains the urethral and vaginal openings4.
While there is often confusion due to the general use of the term “vagina” to refer to the vulva, these are both distinct anatomical structures with different functions. It is therefore essential to understand and use these terms accurately to communicate effectively about reproductive health.
HPV-related cancers
Cervical cancer
Cervical cancer is among the world’s most common cancers in women and people with a cervix5. In the UK, there are around 9 new cases of cervical cancer every day, and it is responsible for nearly 850 deaths per year6. Cervical cancer is the most well-known HPV-related cancer, as it is almost always caused by persistent infection with high-risk HPV, principally types 16 and 187, accounting for 99.8% of all cases. Persistent infection with high-risk HPV can occasionally result in abnormal cells (pre-cancerous lesions) in the cervix, which can subsequently develop into cervical cancer over time if left untreated. It is therefore vital to attend regular cervical screening, in addition to receiving HPV vaccination, for the effective prevention of cervical cancer.
Vaginal cancer
This is a rare type of cancer that starts in the vagina and affects around 250 people in the UK every year. HPV infection is found in a significant proportion of cases, accounting for approximately 75% of vaginal cancers8. Vaginal cancer does not usually cause any symptoms, especially during the early stages, meaning that detection sometimes happens incidentally during routine cervical screening. This highlights the vital role of regular cervical screening in helping with the early detection and management of vaginal cancer cases when treatment is usually much more effective and successful – as with most if not all, types of cancers.
Vulval cancer
This is a relatively rare type of cancer that specifically affects the vulva. There are around 1,400 new cases diagnosed every year in the UK, and approximately 70% of them are caused by HPV infections9. Similar to cervical and vaginal cancer, it is crucial to understand the connection between HPV and vulval cancer in order to be able to take effective preventative measures against infection and help reduce the overall risk of cancer development.
Conclusion
In summary, knowledge serves as a cornerstone in healthcare, because it directs critical factors that can improve overall health outcomes. Gaining a clear understanding of the differences between the cervix, vagina, and vulva is crucial for informed discussions concerning women’s health. Moreover, being aware of the different types of cancer that can specifically affect women, as well as recognising the possible impact of HPV on women’s health, highlights the significance of taking a proactive approach towards prevention through measures such as risk avoidance, HPV vaccination, and regular cervical screening. Armed with the right knowledge, it will help empower women to prioritise their health because recognising symptoms and knowing when to seek medical advice are critical for reducing the risk of developing serious, and sometimes life-changing health conditions.
10zyme: Advancing women’s health
We’re developing a groundbreaking self-test with instant results to detect the main cause of cervical cancer: high-risk HPV. Detecting infections early prevents cancer ever developing.
By enabling self-testing, we aim to empower women, overcome stigma and anxiety, and help eliminate a disease killing hundreds of thousands a year globally. See our Education Section to find out more.
Please follow and support us on social media: LinkedIn, Instagram, and TikTok.
References:
-
- National Cancer Institute. Reproductive system. (Online). Available at: https://www.cancer.gov/publications/dictionaries/cancer-terms/def/reproductive-system [Accessed 07/03/2024]
- Rosner, J. Samardzic, T. Sarao, MS. (2024). Physiology, Female Reproduction. StatPearls Publishing. (Online). Available at: http://www.ncbi.nlm.nih.gov/books/NBK537132/ [Accessed 04/03/2024]
- Jo’s Cervical Cancer Trust. (2020). The cervix. (Online). Available at: https://www.jostrust.org.uk/information/cervix/about-the-cervix [Accessed 07/03/2024]
- Gold, JM. Shrimanker, I. (2023). Physiology, Vaginal. StatPearls Publishing. (Online). Available at: https://www.ncbi.nlm.nih.gov/books/NBK545147/ [Accessed 07/03/2024]
- Kombe, AJK. Li, B. Zahid, A. Mengist, HM. Bounda, GA. Zhou, Y. Jin, T. (2021). Epidemiology and Burden of Human Papillomavirus and Related Diseases, Molecular Pathogenesis, and Vaccine Evaluation. Frontiers in Public Health, 8: 552028. (Online). Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7855977/ [Accessed 03/03/2024]
- Cancer Research UK (CRUK). (2015-2019). Cervical cancer statistics. (Online). Available at: https://www.cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/cervical-cancer [Accessed 07/03/2024]
- Choi, S. Ismail, A. Pappas-Gogos, G. Boussios, S. (2023). HPV and Cervical Cancer: A Review of Epidemiology and Screening Uptake in the UK. Pathogens. 12(2):298. (Online). Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9960303/ [Accessed 07/03/2024]
- Cancer Research UK (CRUK). (2015). Vaginal cancer risk. (Online). Available at: https://www.cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/vaginal-cancer/risk-factors [Accessed 07/03/2024]
- Cancer Research UK (CRUK). (2015-2018). Vulval cancer statistics. (Online). Available at: https://www.cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/vulval-cancer [Accessed 07/03/2024]




One thought on “Women’s Health: Understanding Cancers of the Female Reproductive System”